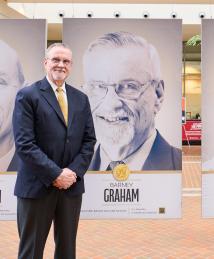
Barney Graham
"My hope is that we can open doors for the next generation of young people who can solve the problems we didn't solve during our generation."
Immunologist and virologist Barney Graham and structural biologist Jason McLellan used structure-based vaccine design to stabilize and modify surface proteins of viruses. They successfully applied their discoveries to the development of COVID-19 vaccines, contributing to billions of vaccine doses administered worldwide since 2020. The first vaccines approved for respiratory syncytial virus (RSV) are also based on their work.
Graham was born in Kansas City, Missouri, in 1953 and grew up in Olathe, Kansas, with parents and grandparents he described as “great role models [who] were hardworking, community service-minded people.” He enjoyed playing football, basketball and baseball with his neighborhood friends, and he developed a lifelong love of mathematics.
At Rice University, Graham earned his bachelor’s degree in biology in 1975, followed by his medical doctorate from the University of Kansas School of Medicine in 1979. Initially, he trained to be a clinician rather than a researcher. “In 1982 and 83, I was chief resident at [Nashville] General Hospital when we had the first AIDS patient in Tennessee come through our doors,” Graham recalled. “It was quite a dramatic thing to see what happened over the next couple of years with HIV and AIDS. So I decided I wanted to specialize in infectious diseases, virology and immunology.”
While he was studying RSV at Vanderbilt University, where he would earn his doctorate in microbiology and immunology in 1991, Graham learned about the shape-shifting properties of fusion proteins. Found on the outer shells of some viruses, these proteins assume different shapes before and after they latch onto healthy cells and create the entry pathway for the virus. The strength of an immune response can differ significantly, depending on which version of the fusion protein antibodies recognize. Graham’s work on RSV would later prove foundational to advancing structure-based vaccine design.
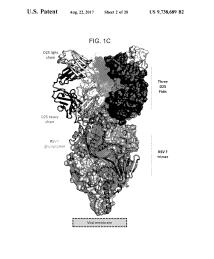
In 2001, Graham joined the National Institutes of Health (NIH) as chief of the viral pathogenesis laboratory and clinical trials core at the National Institute of Allergy and Infectious Diseases. Here, he began collaborating with McLellan in 2008. McLellan had begun his postdoctoral research under Peter Kwong, who had been attempting to develop a structure-based vaccine for HIV. At Graham’s suggestion, they applied this approach to RSV. They isolated and constructed 3D atomic models of the RSV fusion protein and discovered that if they locked the F protein into its prefusion form, the proteins would elicit an antibody response with much stronger neutralizing activity. Their subsequent work influenced the NIH Vaccine Research Center's shift in focus toward a more intentional approach to designing vaccines against emerging viruses that could trigger pandemics.
In 2013, Graham and McLellan began focusing on coronaviruses to extend their findings in RSV to another family of enveloped viruses with similar entry mechanisms. They initially focused on MERS CoV, which had emerged in 2012 while the RSV breakthrough was occurring. However, solving the spike protein structure of the MERS CoV was elusive. At the time, one of Graham’s postdoctoral students had returned from Saudi Arabia with a respiratory infection, and Graham’s analysis detected HKU1, a coronavirus that causes the common cold. Turning their attention to the HKU1 spike resulted in the first spike structure of a human coronavirus. McLellan’s team determined that the addition of two residues of proline, an amino acid known for its rigidity, stabilized the spike protein in its prefusion form. The researchers called this strategy the 2P mutation.
Graham's lab had begun working with Moderna in 2016 on Zika virus vaccines and in 2017 began a strategy to more effectively respond to new pandemic threats by combining precision vaccine antigen design with rapid manufacturing. Focusing initially on paramyxoviruses and coronaviruses, by 2019 they had shown prototype vaccines for both virus families were effective in animal models, and plans were made to test the Nipah virus vaccine (the paramyxovirus prototype) in humans. However, in January 2020, they adjusted their plans to respond to the coronavirus known as COVID-19. By February 2020, Graham, McLellan and their teams had applied the 2P mutation to stabilize the SARS-CoV-2 spike protein, and by March started the first COVID-19 vaccine phase 1 clinical trial with Moderna. Their protein design was incorporated into all the COVID-19 vaccines licensed for use in the U.S., including the mRNA vaccines authorized for human use in late 2020 by Pfizer-BioNTech and Moderna. These vaccines direct a person’s cells to make a viral spike protein and evoke an immune response without ever having been exposed to the virus. If the person is later exposed to the virus, their immune system will recognize and attack it before it can infect healthy cells and cause illness.
In 2023, the Food and Drug Administration approved the RSV vaccine Arexvy®, which used Graham and McLellan’s research to stabilize the fusion protein and enable the body to develop strong antibodies against it. Their stabilizing mutations show promise for other vaccines and could help accelerate the development of new vaccines in response to as-yet-unknown strains and varieties of infectious agents.
Graham’s many honors include the Samuel J. Heyman Service to America Medal for Federal Employee of the Year and the Albany Prize in Medicine and Biomedical Research in 2021, the National Academy of Sciences John J. Carty Award for the Advancement of Science in 2022 and the International Vaccine Institute-SK Bioscience Park MahnHoon Award, which he shared with McLellan in 2024. He serves as professor of medicine and microbiology, biochemistry and immunology and Director of the David Satcher Global Health Equity Institute at Morehouse School of Medicine in Atlanta, and is a member of the National Academy of Sciences. He is dedicated to improving equity in opportunities to train and conduct research, as well as in access to the benefits of research including the equitable distribution of manufacturing capabilities.
“I had the privilege and freedom to explore my own ideas because I ended up in systems that supported me,” Graham explained. “However, there are a lot of talented people who never have the chance to develop to their full potential and achieve their God-given purpose. Based on my experience, there are people from all walks of life and backgrounds who could have done the things I’ve done if they had the opportunity, and that's what I want to focus on the rest of my career. I think we lose out on a lot of talent by not letting some groups of people get their foot in the door. Right now, the world needs all its talent to solve the problems we have.”